Bowel Cancer

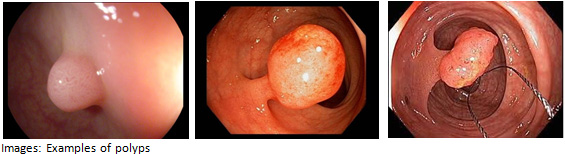
Bowel cancer refers to both colon and rectal cancer (that is, cancer that occurs anywhere in the large intestine, including the rectum). It is also often referred to as “colon cancer” or “bowel cancer”. According to the Australian Government Department of Health official statistics, more than 14,000 Australians were diagnosed with bowel cancer in 2015. Bowel cancer remains the second leading cause of cancer-related death in Australia. This is surprising as bowel cancer can be prevented, by regular routine screening and removal of silent small, benign polyps (growths). Early detection is the key, and people with early stages of bowel cancer can be successfully treated. Recent international studies have shown that more than 90% of people diagnosed with stage 1 cancer (confined to the colon or rectum), survive more than five years.
DEVELOPMENT OF BOWEL CANCER
ADVANTAGES IN DETECTING EARLY STAGE CANCER
As with any cancer, bowel cancer is classified into “stages” that describe the extent of the spread of cancer in the body. This “staging” depends on how deep the cancer has grown into the walls of the colon, if the lymph nodes near the cancer contain cancerous cells, or if the cancer has spread into the other organs (most commonly the liver and lungs). Staging is a combination of physical examination, imaging tests (typically Ultrasound, CT scanning +/- MRI/PET scans) and histopathology. The stage is essential in determining treatment options and can have profound impacts on long term prognosis.
Bowel cancer is generally staged on a scale from 0 to IV – as follows:
- Stage 0: Cancer cells are found in the mucosa (innermost layer) of the bowel wall. These abnormal cells may become cancer and spread (Stage 0 is also referred to Carcinoma in Situ).
- Stage I: Cancer has formed in the mucosa (innermost layer) of the colon wall and has spread to the sub-mucosa (layer of tissue under the mucosa). Cancer may have spread to the muscle layer of the colon wall. Survival is very likely for stage I (91%).
- Stage II: Cancer has spread through the muscle layer of the bowel wall to the serosa (outermost layer) of the bowel wall; or to nearby organs. Patients can expect a survival rate of 80% for stage II bowel cancer.
- Stage III: Cancer may have spread through the mucosa (innermost layer) of the colon wall to the sub-mucosa (layer of tissue under the mucosa); or to the muscle layer of the colon wall; to nearby lymph nodes. The survival rate at this stage is around 65%.
- Stage IV: Also known as “metastatic”, “advanced” or “secondary” bowel cancer. In this advanced stage, cancer may have spread through the colon wall and may have spread to nearby organs or lymph nodes; and to one organ that is not near the colon (such as the liver, lung, or ovary, or to a distant lymph node).
RISK FACTORS FOR BOWEL CANCER
Both inherited and lifestyle factors appear to play a part in the development of colon polyps and bowel cancer.
It should be noted however, that the majority of people who develop polyps and cancer don’t have any obvious risk factor. The vast majority of patients (90%) with bowel cancer are above the age of 50. It is for this reason that many experts emphasize the importance of routine bowel cancer screening every 5-10 years if you are between the 50-80 age group.
There are some individuals who have a higher than average risk of developing bowel cancer (up to 1:10), including:
- Family history – a parent, brother, sister, son or daughter who has/had cancer of the colon;
- An individual who has/had colon polyps;
- An individual who has/had inflammatory bowel disease such as Crohn’s Disease or Ulcerative Colitis.
If you have multiple risk factors for bowel cancer, it is likely that you may require a colonoscopy from a younger age or a shorter interval between examinations.
WHAT ARE THE SYMPTOMS
It should be pointed out that a person over the age of 50 should not wait until symptoms develop. Small polyps do not bleed, not all large polyps bleed and when a polyp bleeds, the bleeding can be erratic. Symptoms of bowel cancer may vary from person to person, but it’s important to understand that there may be no signs at all, particularly when the cancer is very deep inside the colon. Experts recommend that if you’ve reached 50, getting a colonoscopy is important even when you have no symptoms.
By the time a person begins experiencing symptoms associated with a large polyp, the polyp may have turned cancerous. On the other hand, if you experience the symptoms which can be associated with bowel cancer, remember that you don’t necessarily have bowel cancer. Common symptoms include:
- Rectal bleeding. The blood could be dark or altered, but can also be fresh looking. Rectal bleeding in people over the ageof 50 should always be investigated with colonoscopy. “Faecal Occult Blood Test” or FOBT (see below) is not an appropriate test in this scenario.
- Mucous in bowel motions. Although mucous in the stools in people between the ages of 20-40 are often associated with Inflammatory Bowel Disease (Crohn’s Disease or Ulcerative Colitis), but mucous can also occur in bowel cancer.
- Abdominal pain, which can be non-specific.
- Anaemia on routine blood testing or annual check up, particularly if your doctor notes the low Iron levels in the blood. When bowel cancer causes anaemia, it is a late sign and should always be investigated further although there are many causes of anaemia which are benign. Common benign causes include menorrhagia (abnormal and prolonged menstruation cycles).
- Change of bowel habits (new onset of constipation or loose stools)
- Weight loss or weakness.
In general, a polyp doesn’t cause any initial symptoms, but if you experience any of these signs, please discuss them with your doctor immediately. Your doctor can determine your level of risk and proceed with the proper course of action.
Faecal Occult Blood Test (FOBT)
An FOBT is not recommended for those who have symptoms such as bleeding etc.
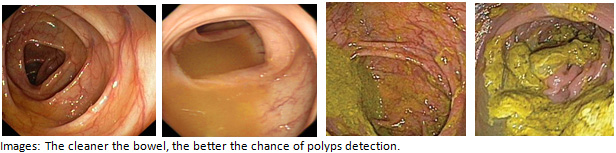
Faecal Occult Blood Test is a useful tool in screening for bowel cancer in patients over the age of 50. It is not as accurate as a colonoscopy, but can be useful if done every 1-2 years as it is simple and non-invasive, particularly if you have had a normal colonoscopy within the last 2-3 years. It tests for minute traces of blood in the stools, but remember that not all large polyps bleed and hence the test can be falsely negative. FOBT is recommended for all Australians (regardless of ethnic background) every 1-2 years for those:
- Aged 50 and over AND
- With no symptoms (that is, if you have rectal bleeding and aged over 50, FOBT is not the right test and it is appropriate and highly recommended that you have a colonoscopy) AND
- With no family history of bowel cancer or polyps.
HOW CAN BOWEL CANCER BE PREVENTED
Bowel cancer can be prevented by removing pre-cancerous polyps or abnormal growths in the colon before they develop into cancer. Doctors and medical researchers continue to discover more about colon cancer and the factors that influence its development. As knowledge increases, more effective screening tools are developed to help detect the disease in its early stages. The state-of-the-art and most accurate prevention tool is a colonoscopy. Estimates show that with simple lifestyle changes and widespread routine screening, many of new cases of bowel cancer in Australia could be prevented. However, despite the fact that screening methods, including colonoscopy, are very effective and with the available results from international studies, bowel cancer screening remains under-utilised and lags far behind screening for breast and cervical cancers.
For further advice and information, you can request an appointment, or call one of our receptionist team on Rosebud Endoscopy .